Different modified live vaccines (MLV) are available in the market for both PRRSV-1 and PRRSV-2. Which should we use to successfully control PRRS in regions where there’s coinfection?
The co-existence of both PRRSV-1 and PRRSV-2 at individual and herd level has been increasingly reported in several Asian countries, including China, Korea, and Vietnam (Chen et al., 2011; Kim et al., 2011) and also in some European countries such as Denmark and Germany.
Different modified live vaccines (MLV) are available in the market for both PRRSV species so it is difficult to justify which species of PRRSV MLV should be used to successfully control PRRS in the region where the coinfection does exist.
UNISTRAIN® PRRS is the live attenuated vaccine based on PRRSV1 from HIPRA, commercially available in both intramuscular (IM) and intradermal (ID) administration applied by Hipradermic®.
UNISTRAIN® PRRS administered IM, has already demonstrated partial protection against heterologous PRRSV1 (Bonckaert et al., 2016) or PRRSV2 (Roca et al., 2012).
However, UNISTRAIN® PRRS had not been evaluated yet against the coinfection of PRRSV1 and PRRSV2 at the same time.
On the other hand, there are not any report on the induction of immune response, IL-10 production and protective efficacy of the vaccine administered ID in these circumstances.
IL-10 is a cytokine that functions in immunoregulation. In PRRSV infection, IL-10 levels are reportedly associated with severity of clinical disease (van Reeth and Nauwynck, 2000) and can delay the immune response.
Therefore the objectives of the present study were investigate the immune response of pigs vaccinated IM or ID with UNISTRAIN® PRRS, evaluate the protective efficacy against challenge with HP-PRRSV2 (Thai strain) alone or in coinfection with PRRSV1 and learn more about safety of the vaccine by evaluation of IL-10 production as it can delay the immune response.
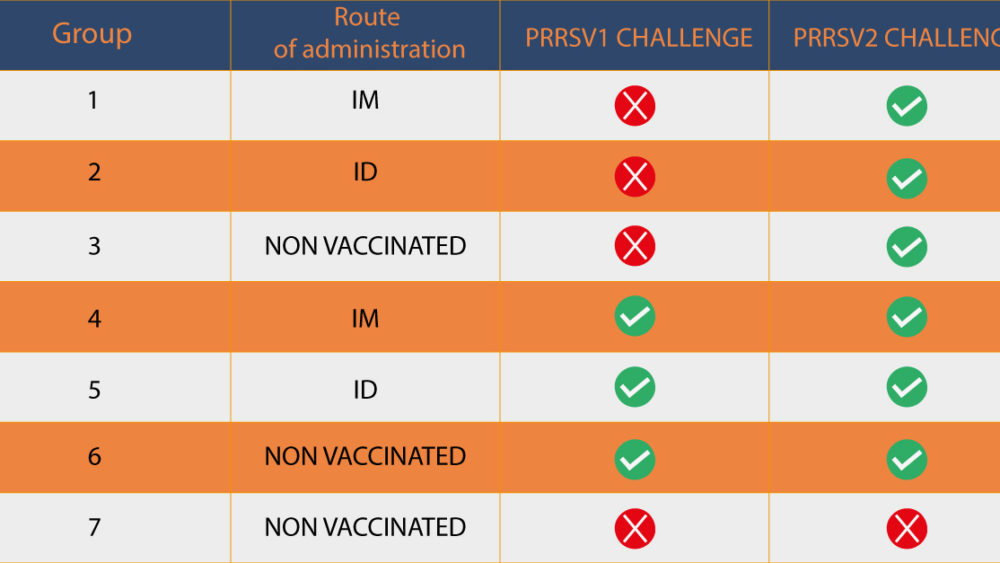
Forty-two, 3-week-old, PRRSV-free pigs were allocated into 7 groups as shown in Table 1.
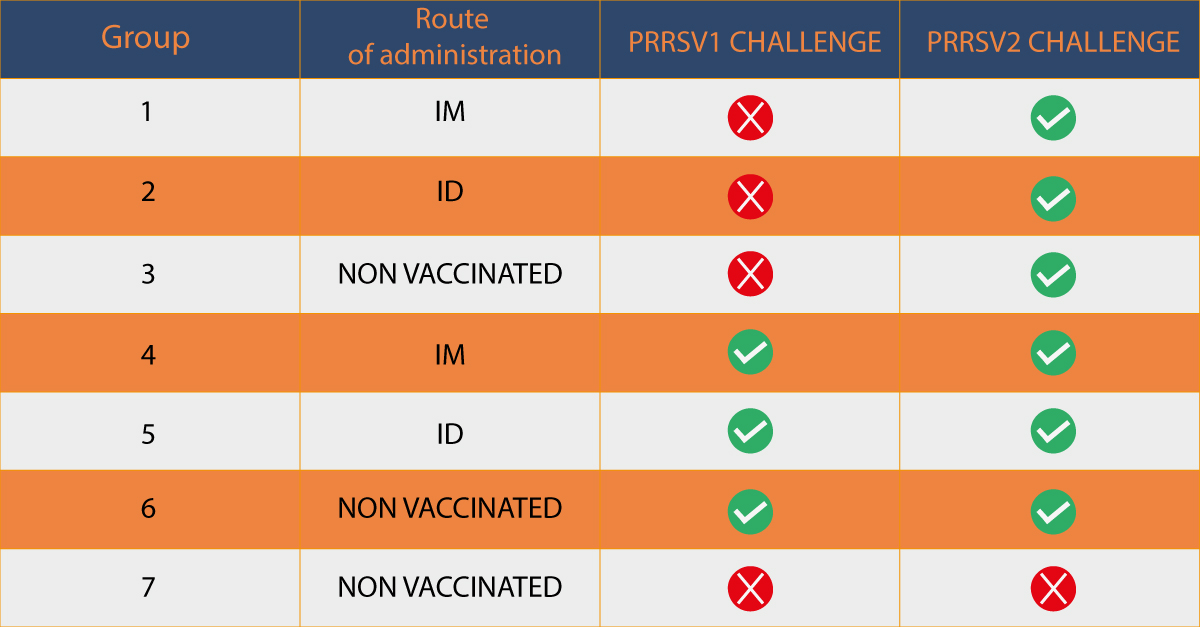
Following vaccination and challenge, pigs were monitored for PRRSV quantification by RT-qPCR, safety of the vaccine by IL-10, immune response including ELISA (IDEXX PRRS X3 Ab test) and IFN-γ-PC (ELISPOT assay) and macroscopic lung lesions as shown in Figure 1.
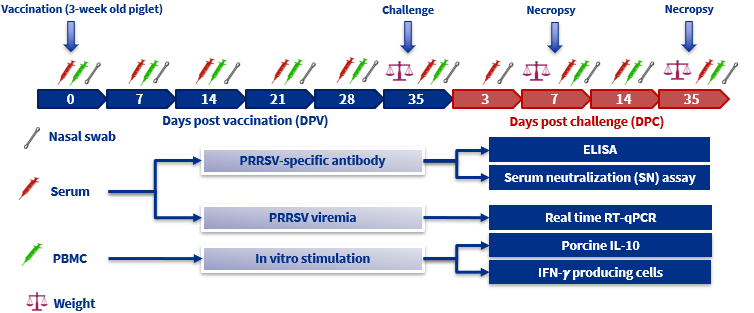
FIGURE 1: Experimental design showing UNISTRAIN® PRRS administration details and sampling time points. PBMC: Peripheral blood mononuclear cells. IFN-γ: Interferon-γ-secreting cells.
Results:
1. Reduced clinical disease, viremia and shedding in vaccinated animals
All vaccinated pigs showed no systemic adverse reactions (no fever and no respiratory disease associated with PRRSV) after vaccination and less severe clinical disease than the non-vaccinated ones after the challenge.
The IM and ID vaccinated with UNISTRAIN® PRRS groups showed reduced PRRSV viremia and no nasal shedding following vaccination. After challenge although IM groups showed higher viremia and shedding than the ID groups, in all the vaccinated groups, viremia and shedding were lower compared to the non-vaccinated ones.
2. IM and ID vaccination induced similar antibody response as measured by ELISA and SN assay
Regardless of the route of vaccination and PRRSV isolates of recall antigen used, an increased PRRSV specific antibody response were firstly detected in the vaccinated groups with ELISA at 7 days post vaccination (DPV), with levels above the cut-off level from 14 to 35 DPV and at 21 DPV with SN assay. All the results were significantly higher (P<0.05) than those of the non vaccinated groups throughout the experiment.
Moreover, animals vaccinated with UNISTRAIN® PRRS showed cross-neutralizing antibodies at 21 DPV. Neutralizing antibodies levels were higher in the ID group challenged with the homologous strain (3rd-4th week post vaccination) compared to the IM group.
3. ID vaccination induced lower IL-10 production than IM vaccination
The induction of IL-10 production was different between vaccinated groups. Two weeks of delay was observed in the ID vaccinated pigs compared to the IM groups, with the first detection at 21 DPV.
Higher levels were found in the IM vaccinated groups at 7, 14, 28, and 35 DPV. (Figure 2).
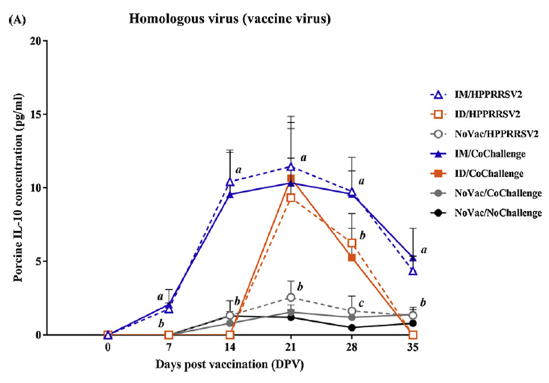
Figure 2: Quantification of IL-10 in the supernatant of stimulated PBMC with the vaccine strain following vaccination.
4. ID vaccination induced higher IFN-γ-SC than IM vaccination
IFN-γ-SC were first detected in the ID vaccinated groups at 28 DPV and continuously increased, reaching the highest levels at 35 DPV. In contrast, IFN-γ-SC were first detected in the IM vaccinated groups at 35 DPV.
After the challenge, vaccinated animals had higher titers of IFN-γ-SC compared to non-vaccinated animals and in almost all the cases, the ID vaccinated groups showed higher titers compared to the IM vaccinated groups. (Figure 3).
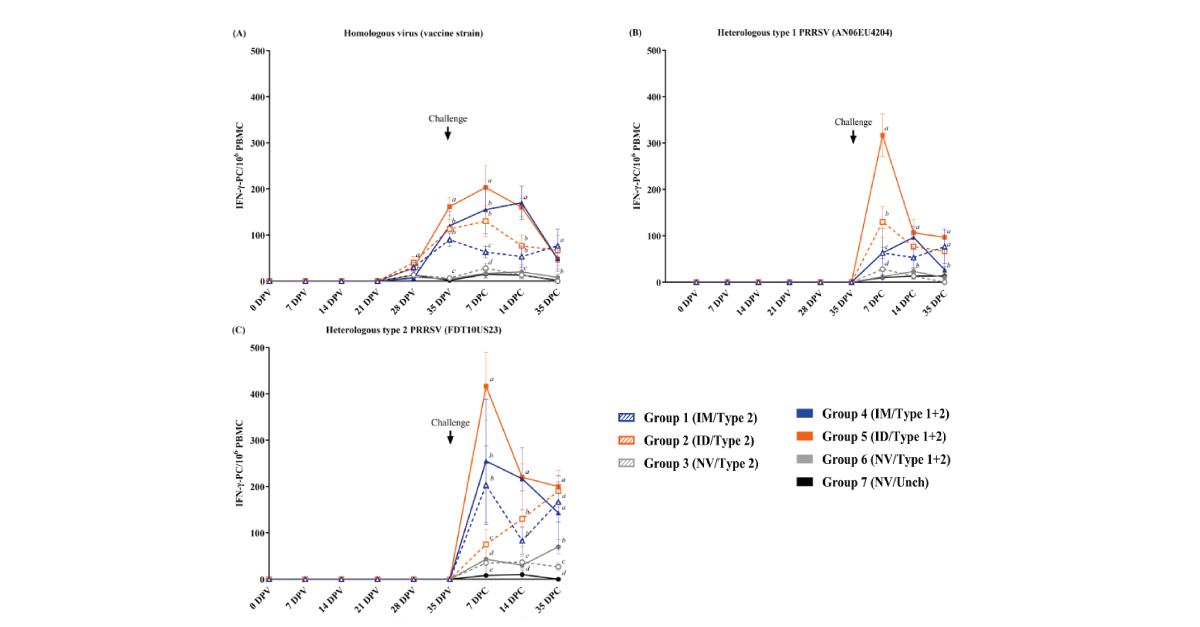
Figure 3: Evaluation of PRRSV-specific IFN- γ -secreting cells (SC) after stimulation with (A) homologous virus (vaccine virus), (B) heterologous PRRSV1 (AN06EU4204) and (C) heterologous HP-PRRSV2 (FDT10US23). Values are expressed as the mean±SEM.
5. IM and ID vaccination reduced macroscopic and microscopic lung lesions following challenge
Following challenge with HP-PRRSV2, either alone or co-challenge with PRRSV1, PRRSV lung lesions, both microscopically (Figure 5) and macroscopically (Figure 6), were significantly reduced in vaccinated pigs than that of non vaccinated pigs, regardless to the route of vaccine administration.
It is notably that ID vaccinated pigs had significantly lower levels of lung lesion scores than that of IM vaccinated pigs.
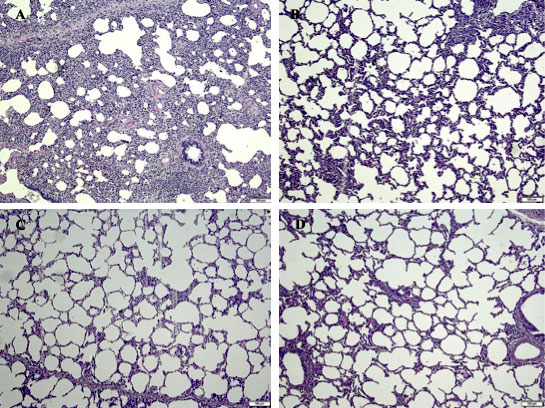
Figure 5: Microscopic lung lesions following challenge of the (A) non vaccinated/challenged, (B) IM vaccinated pigs, (C) ID vaccinated pigs and (D) non vaccinated/non challenge pigs. H&E staining. Bar =100 μm.
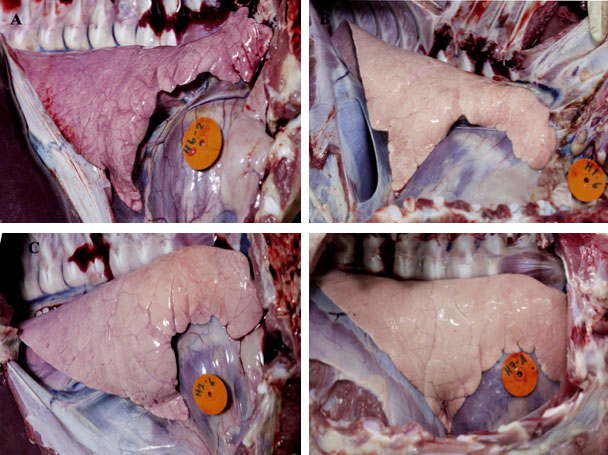
FIGURE 6: Macroscopic lung lesions following challenge at 7 DPC of the (A) non vaccinated/challenged, (B) IM vaccinated pigs, (C) ID vaccinated pigs and (D) non vaccinated/non challenge pigs.
Conclusions
The results of the study suggested that:
1. Vaccination with UNISTRAIN® PRRS, either by IM or ID, can induce humoral and cell-mediated immune responses.
Genetic similarity between the vaccine and field virus is not a good indicator of the protective efficacy provided by a PRRSV MLV vaccine (Opriessnig et al., 2002).
The protective efficacy of a PRRSV MLV is usually determined by the reduction in viremia and lung lesions following challenge with virulent viruses (Labarque et al., 2003). Therefore, vaccine mediated reduction of PRRSV viremia is critical for controlling the infection pigs.
2. UNISTRAIN® PRRS administered by either IM or ID can provide partial heterologous protection against challenge with HP-PRRSV-2, either alone or in conjunction with PRRSV-1, as demonstrated by reduced lung lesions and viremia.
The advantages of the ID administration by a needle-less device are that it is less invasive, painless, safe, quick and easy.
Furthermore, the ID administration could induce a stronger cellular response compared to the IM due to the delivery through the intradermal route could induce T cell polarization favoring the induction of IFN-γ.
This phenomenon was evident in the present study. Another possibility of higher IFN-γ-SC in ID vaccinated pigs could be due to the lower IL-10 levels.
Our results demonstrated that the IL-10 production was delayed and lower in ID vaccinated pigs.
In conclusion, the ID route might represent an alternative to improve vaccine efficacy, as it induced lower IL-10 levels and more IFN-γ-SC.
References
Madapong,A; et al. Immune response and protective efficacy of intramuscular and intradermal vaccination with porcine reproductive and respiratory syndrome virus 1 (PRRSV-1) modified live vaccine against highly pathogenic PRRSV-2 (HP-PRRSV-2) challenge, either alone or in combination with of PRRSV-1, Veterinary Microbiology, Volume 244, 2020.
HIPRA © All rights reserved